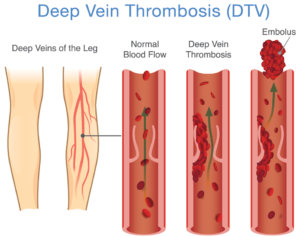
Deep Vein Thrombosis
What is Deep Vein Thrombosis?
Deep vein thrombosis can develop if you’re sitting still for a long time, such as when traveling by plane or car, or if you have certain medical conditions that affect how your blood clots.
Deep vein thrombosis is a serious condition because a blood clot that has formed in your vein can break loose, travel through your bloodstream and lodge in your lungs, blocking blood flow (pulmonary embolism).
Deep vein thrombosis occurs when a blood clot forms in the veins that are deep in your body, often in your legs. Blood clots can be caused by many different things — namely anything that causes your blood not to circulate normally or clot properly.
Symptoms
In about half of all cases, deep vein thrombosis occurs without any noticeable symptoms. When deep vein thrombosis symptoms occur, they can include:
- Swelling in the affected leg, including swelling in your ankle and foot.
- Pain in your leg; this can include pain in your ankle and foot. The pain often starts in your calf and can feel like cramping or a charley horse.
- Warmth over the affected area.
- Changes in your skin color, such as turning pale, red or blue.
When to see a doctor
If you develop signs or symptoms of deep vein thrombosis, contact your doctor for guidance.
If you develop signs or symptoms of a pulmonary embolism — a life-threatening complication of deep vein thrombosis — seek medical attention immediately.
The warning signs of a pulmonary embolism include:
- Unexplained sudden onset of shortness of breath
- Chest pain or discomfort that worsens when you take a deep breath or when you cough
- Feeling lightheaded or dizzy, or fainting
- Rapid pulse
- Sweating
- Coughing up blood
- A sense of anxiety or nervousness
Risk Factors
Many factors can increase your risk of developing deep vein thrombosis (DVT), including:
- Sitting for long periods of time, such as when driving or flying. When your legs remain still for long periods, your calf muscles don’t contract, which normally helps blood circulate. Blood clots can form in the calves of your legs if your calf muscles aren’t moving. Although sitting for long periods is a risk factor, your chance of developing deep vein thrombosis while flying or driving is relatively low.
- Inheriting a blood-clotting disorder. Some people inherit a disorder that makes their blood clot more easily. This inherited condition may not cause problems unless combined with one or more other risk factors.
- Prolonged bed rest, such as during a long hospital stay, or paralysis. When your legs remain still for long periods, your calf muscles don’t contract to help blood circulate, which can make blood clots develop.
- Injury or surgery. Injury to your veins or surgery can slow blood flow, increasing the risk of blood clots. General anesthetics used during surgery can make your veins wider (dilate), which can increase the risk of blood pooling and then clotting.
- Pregnancy. Pregnancy increases the pressure in the veins in your pelvis and legs. Women with an inherited clotting disorder are especially at risk. The risk of blood clots from pregnancy can continue for up to six weeks after you have your baby.
- Cancer. Some forms of cancer increase the amount of substances in your blood that cause your blood to clot. Some forms of cancer treatment also increase the risk of blood clots.
- Inflammatory bowel disease. Bowel disease, such as ulcerative colitis, increases your risk of DVT.
- Heart failure. People with heart failure are at risk of DVT because a damaged heart doesn’t pump blood as effectively as a normal heart does. This increases the chance that blood will pool and clot.
- Birth control pills or hormone replacement therapy. Birth control pills (oral contraceptives) and hormone replacement therapy both can increase your blood’s ability to clot.
- A pacemaker or a thin, flexible tube (catheter) in a vein. These medical treatments can irritate the blood vessel wall and decrease blood flow.
- A history of deep vein thrombosis or pulmonary embolism. If you’ve had DVT before, you’re more likely to have DVT in the future.
- A family history of deep vein thrombosis or pulmonary embolism. If someone in your family has had DVT or a pulmonary embolism, your risk of developing DVT is increased.
- Being overweight or obese. Being overweight increases the pressure in the veins in your pelvis and legs.
- Smoking. Smoking affects blood clotting and circulation, which can increase your risk of DVT.
- Age. Being over age 60 increases your risk of DVT, though it can occur at any age.
- Being tall. Taller men may be more likely to have blood clots. Taller women do not appear to have an increased risk, perhaps because most women do not typically get as tall.
Diagnosis
To diagnose DVT, your doctor will ask you about your symptoms and perform a physical exam so they can check for swelling, tenderness, and discoloration on your skin. In addition, they may look for blood clots via a blood test, CT or MRI scan, ultrasound, or venography, which involves injecting a dye into a large vein in your foot and ankle.
Treatments
The goal of DVT treatments is to prevent your blood clot from increasing, breaking loose, and causing a pulmonary embolism, which occurs when one or more arteries in your lungs become blocked by a blood clot. Blood thinners, clot busters or thrombolytics, filters, and compression stockings are all viable treatment options.
If you would like to schedule an appointment at Preferred Vascular Group to have a consult with a Board-Certified physician or would like to have one of our highly trained care providers reach out to you, please click on a button below: